Systematizing Equity: How Healthcare Organizations Can Turn Good Intentions Into Meaningful Action
Race, income and other social factors have a profound effect on patient health. A growing wave of research and public awareness is moving healthcare organizations to acknowledge these factors and work toward providing more equitable care.
But change is tricky.
“Addressing inequities takes a combination of personal skills and tangible frameworks, which help you get to the bottom of some really thorny issues,” says Nate Higby, an improvement specialist at Virginia Mason Franciscan Health.
Higby and others have helped create and establish new tools and practices at the organization that help leaders and teams apply an equity lens to their work and decisions. These can inspire other organizations who want to do the right thing but don’t know how.
“The goal of these tools is to systematize equity by integrating equity conversations and considerations in daily decision making and process improvement,” says Higby.
Health Inequities Have Deep Roots and Serious Consequences
Health and healthcare in the U.S. vary widely depending on where you live and who you are. Zip codes with higher poverty rates and levels of racial segregation tend to have lower life expectancy than areas that are more integrated and affluent. Other studies have shown that breast cancer leads to higher mortality rates among Black women than White women, despite similar incidence rates.
“There’s no doubt that improving health equity can improve health — on a dramatic scale,” says improvement specialist Shawna Whipple.
For example, new recommendations for diagnosing kidney disease could mean a million Black Americans receive treatment earlier in their disease instead of waiting for it to progress. Prior recommendations were built on a racist assumption that Black people have higher muscle mass and kidney function than other people, so their kidney function could afford to deteriorate more before intervention was necessary. But many recent studies have exposed the bias in that assumption and the high burden of disease it places on the Black population. As a result, in September 2021, the National Kidney Foundation and the American Society of Nephrology outlined a new, “race-free” approach to testing and diagnosis.
“Following these new guidelines is just one of the changes we’ve made to enhance equity,” Whipple says.
Enhancing Equity Requires Full Commitment and a Rigorous Approach
Virginia Mason Franciscan Health intensified its focus on equity in 2020, in response to that year’s Black Lives Matter marches and nationwide calls for social reform. Team members at all levels echoed those calls, urging the organization to take clear and meaningful action to improve equity for patients and workers.
To give equity the necessary attention and rigor, Virginia Mason’s process improvement team knew they wanted to build on the Virginia Mason Production System® — the management method already in use throughout the organization. Still, they faced a difficult question, one familiar to many organizations: How exactly do we change?
“We started by conducting a weeklong workshop involving a multiracial, multidisciplinary group of employees,” Higby explains. The workshop also included a patient participant and additional patient perspectives were included through gathered feedback. Based on this workshop, the team created several equity tools that were then introduced to leaders and team members within the organization and refined over time.
Today, the effort to systematize equity is supported by three main tools:
Equity Pauses
These are breaks in team huddles, planning meetings, and other situations that pause the work at hand in order to view it through an equity lens. During an equity pause, staff may simply ask, “What are the equity implications of this effort that we haven’t discussed or addressed yet?,” or they may consult a toolkit with questions and information about different aspects of equity, such as implicit bias and psychological safety. The idea for this practice came from Dr. Ben Danielson, a physician and community leader in Seattle who has led equity work at other organizations. All frontline staff and clinicians learn about equity pauses in their required onboarding training, and leaders practice these pauses in their required leadership coursework.
“Equity pauses are now standard in all improvement events, and leaders often work them into other meeting agendas and project planning,” says Higby.
Download the Equity Pause Toolkit
The Inequity Waste Wheel
This is a graphic and accompanying impact analysis tool that describes six different types of inequities to help teams identify and prevent them and the harm they cause. Teams may consult this resource as part of an Equity Pause, a team or program meeting, process improvement efforts, or their day-to-day work.
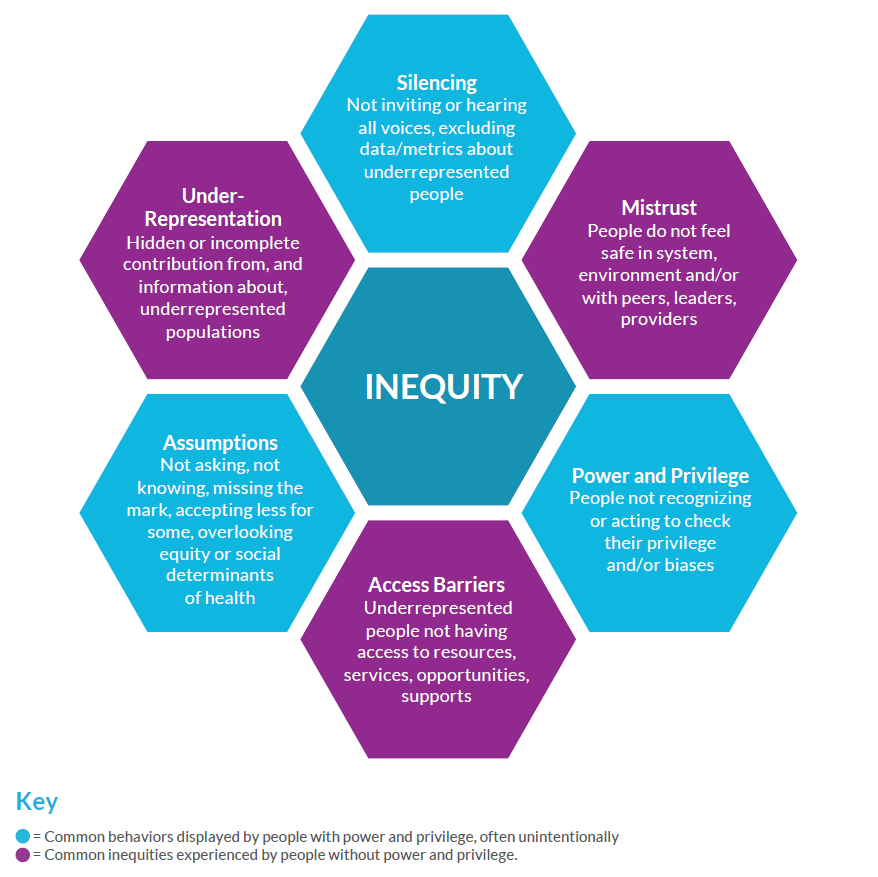
The analysis questions are based on those in the Racial Equity Impact Assessment created by Race Forward: The Center for Racial Justice and Innovation. The Virginia Mason Franciscan Health version connects the questions to the six types of inequity in the waste wheel. Users consider questions such as, “Which racial or ethnic groups, or other under-represented groups, are most advantaged/disadvantaged by the issues this proposal seeks to address?” and “What adverse effects or unintended consequences could result from this proposal?”
“Together, the wheel and questions provide a clear and methodical way of assessing the equity impacts of a decision or process,” says Alice Forsythe, an executive partner at Virginia Mason Institute.
Download the Inequity Waste Wheel Toolkit
The Equity Learning Pathway
This training resource includes videos, podcasts and activities covering eight different equity topics, including privilege, implicit bias and anti-racism. The module is available via the organization’s intranet, and team members can explore it as needed or desired. For example, before leading an improvement event, leaders are prompted to review relevant resources in the pathway to help them keep equity top of mind as they prepare to facilitate equity pauses with their improvement team.
The learning pathway was born in response to survey data from the initial equity improvement workshop, which revealed that many leaders didn’t feel confident applying equity concepts in their work. This metric continues to be tracked as team members pilot the learning pathway.
“We’ve seen a 57.9% improvement in confidence among staff after using resources in the pathway,” says Forsythe.
Observing Impact
Though the tools are new, they have already helped spur two clinical reforms at Virginia Mason Franciscan Health. One is in the transplant department, which removed a longstanding requirement for dental records that the team found was disproportionately excluding candidates of lower socioeconomic status. The second is adopting the new race-free screening recommendations for kidney disease. While more and more organizations are following these recommendations today, Higby says the process at Virginia Mason Franciscan Health was aided significantly by the equity tools they had in place.
“These tools provided the venue and platform for team members to speak up about these issues and helps us escalate them more quickly,” he explains.
Staff have used the Inequity Waste Wheel to get past longstanding communication challenges and other barriers. During one recent improvement event, using the wheel helped teammates have a productive and eye-opening discussion about the challenges that medical assistants and other staff can have when relaying messages from providers to patients. Providers realized that their use of jargon makes those messages hard to understand, while their seniority makes junior teammates feel uncomfortable asking for clarification. The Inequity Waste Wheel helped illuminate these power dynamics and establish a higher level of respect and psychological safety so that teammates can communicate more openly.
More broadly, leaders are encouraged by how teams across the organization are embracing the new tools. Whipple regularly sees the Inequity Waste Wheel graphic displayed in team workstations and production boards. This includes teams that haven’t received specific equity training — demonstrating that the mindset is spreading organically and becoming more routine.
“This is hard work,” Whipple says, “but we’re building momentum. We’re making the difference we know is necessary.”
Download the toolkits
Watch the webinar
Learn more about this work from team members with real experience implementing this approach at Virginia Mason Franciscan Health.





