Case Study | Improving Patient Flow in Primary Care
“I used a leadership stipend to attend the Optimizing Flow in the Ambulatory Setting course at Virginia Mason Institute’s Seattle training facility. I was so inspired by the course that I asked our medical director if I could send the whole team. He agreed to have Virginia Mason Institute come to us at WakeMed to facilitate additional training.”
– Dr. Theresa Amerson, Executive Medical Director of Primary Care
Background
In an effort to better deliver timely patient care, foster more efficient stewardship of clinical resources, and effectively address ongoing staff burnout, WakeMed Health and Hospitals tested and implemented ambulatory flow training across 11 primary care clinics in North Carolina. Executive Medical Director of Primary Care, Theresa Amerson, spearheaded the work and shared her experience, lessons learned and positive outcomes.
Problem
- Of the patients seen each day, 20 percent of patient notes regularly went unfinished each day.
- 44 percent of administrative emails went unread.
- Morning schedules routinely ran into staff’s lunch by an hour leaving only 30 minutes for a desk lunch and in-basket processing.
- Afternoon schedules ran late by 20-30 minutes.
- Staff left the office after 5:00 p.m. without completing all the work for the day.
- An additional 1.5 hours of charting and paperwork remained for providers to complete in the evening.
Approach
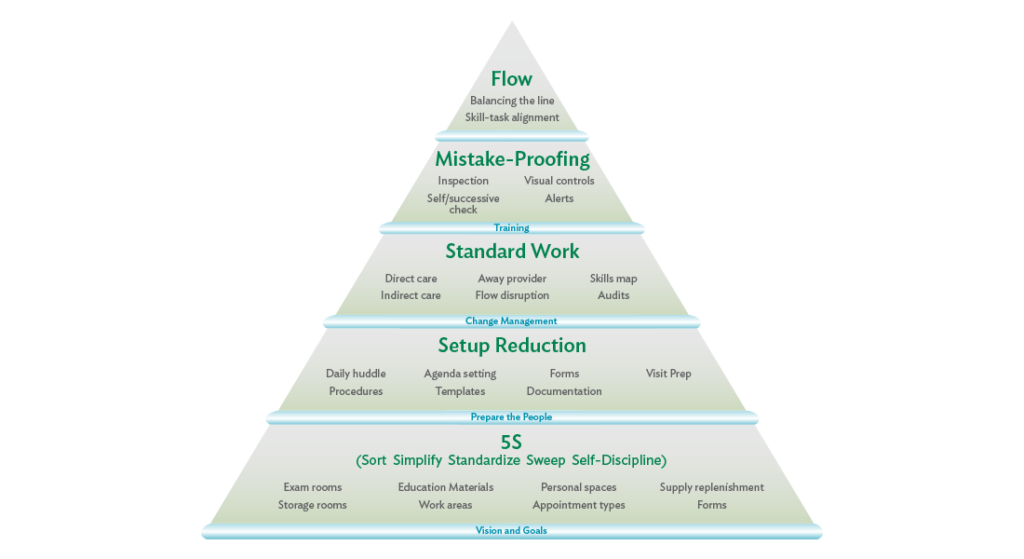
WakeMed included 100 primary care staff members in four Optimizing Flow in the Ambulatory Setting training sessions, facilitated by Virginia Mason Institute lean experts, each two-and-a-half-days long. Four clinics (Downtown Raleigh, Cary Parkway, Knightdale, and Brier Creek) in the WakeMed Health and Hospital Systems were fully trained and successfully implementing flow concepts and tools at the time of this case study. Seven additional clinics were at least 50 percent trained.
“Foundational to the process was the infrastructure building component. We needed to get the operational pieces in place – or Nemawashi – creating standard work.”
– Dr. Theresa Amerson
Progress and milestones during implementation included:
Standard Work: Operations Huddle
Operations-specific huddles take place daily involving the practice manager, clinical staff, front desk staff and providers at the clinic production board. Huddle boards are in use, and notes are being taken and kept on file in the office as part of the practice manager standard work.
5S: Exam Rooms
A 5S agreement is in place for exam rooms. 5S is a strategy used to keep a workplace safe and organized that is the foundation of improving patient flow. All clinic exam rooms now meet Level V, the highest standards distinction in WakeMed’s new flow progress metrics system, to include items kept in the cabinets, drawers, exam tables and desktop areas. Practice manager standard work includes routine 5S agreement audits of these areas and re-education.
5S: Main Supply Area
A 5S agreement is in place for all supply areas and stock rooms. All supply areas and stock rooms meet Level V standards. Practice manager standard work includes routine 5S agreement audits of these areas and re-education occurs regularly, as needed to maintain Level V standards.
Standard Work: Restocking and Ordering Supplies
Room supply restocking in exam and procedure rooms now occurs “just in time” using Kanban, or scheduling, systems. All supply levels are appropriate to ensure zero defects (no supplies are missing when needed). All clinical staff and providers are educated on the restocking and ordering system and participate in maintenance of appropriate par levels. Practice manager standard work includes routine audits or restocking and ordering standard work and par levels.
5S: Workstations
A 5S agreement is in place for all shared workstations and flow stations. All workstations meet Level V standards. Practice manager standard work includes routine 5S agreement compliance checks.
5S: Clinical and Point-of-Care Areas
A 5S agreement is in place for all clinical and point-of-care areas. All clinical and patient care areas meet Level V standards. Practice manager standard work includes routine 5S agreement audits of these areas, and re-education occurs regularly as needed to maintain Level V standards.
Standard Work: Paper Management
Standard work for management of tasks originating on paper are followed to include forms, faxed Rx requests, faxed results, etc. All clinical, non-clinical staff and providers have been trained on the appropriate standard work for paper management. Practice manager standard work includes routine audits to ensure the standard work is utilized and to inquire about any “rocks in shoes” related to this standard work.
Mistake-Proofing: Waste Walks
All team members and providers are engaged in periodic waste walks to evaluate all types of waste in a clinic area or with a clinic process. Information gathered during the waste walk guide the idea forms and plan-do-study-act (PDSA) cycles on the genba.
Setup Reduction: Weekly Improvement Huddles
Improvement-specific huddles take place weekly involving the practice manager, clinical staff, front desk staff and providers.
“Flow has taught us that effective team-based care can restore joy to the workplace.”
– Dr. Theresa Amerson
Outcomes
Implementation and consistent practice around 5S, standard work, and mistake-proofing has resulted in the following performance improvement metrics:
• 100 percent completion of medical notes for all patients seen and walk-in patients are accommodated within 15 minutes
• All in-basket items are processed in flow
• All administrative emails are answered
• Staff enjoyed a full one-hour for lunch without work to do
• All work was completely done by 4:30 p.m.
• Real-life scenarios were collected to create a Practice Manager’s Playbook to enable greater ease coaching others through flow implementation