Case Study | Building a New Outpatient Surgery Center With Patients and Staff in Mind
At a Glance
The Organization
The Orthopedic Outpatient Center is a state-of-the-art facility in southwest Oregon, operated by the Southern Oregon Orthopedics group. The group followed a Lean approach to designing their new facility, in order to control construction costs and optimize care delivery.
Key Decisions
- Developing design concepts and functional narratives to inform the architect’s plans
- Assembling a multidisciplinary group to generate and evaluate ideas
- Breaking with convention to devise innovative solutions for patient flow, storage and other challenges
Key Results
- No change orders, delays or surprise expenses during design and construction
- Patient capacity increased from 20 per day to 50 per day
- OR turnover for back-to-back total knee replacements achieved in less than 20 minutes
The Context
Aging Facilities Cast a Grim Shadow Over Healthcare
The age of physical infrastructure is a widespread problem for healthcare organizations. For example, according to the American Hospital Association, one-third of rural hospital facilities in the U.S. are at least 15 years old on average.
This translates to a range of immediate and downstream costs. Patients and staff must contend with unideal environments and experiences. Old facilities might not accommodate new technology and may run afoul of current building codes and regulations.
The cost of upgrading or rebuilding is also significant. Construction bills run to the millions and billions. Projects commonly start with an architect’s or builder’s design, rather than an organization’s needs, leading to costly change orders and painful sacrifices as organizations figure out how they’ll inhabit their new space. Organizations may even see aging infrastructure hurt their credit rating, making loans and improvements even harder to attain.
The Challenge
Capacity and Care Goals Unattainable in Outdated ASC
Surgeons in the Southern Oregon Orthopedics group had practiced in the ambulatory service center (ASC) of an aging rural hospital for more than 20 years. The group of 12 surgeons shared 5 ORs with many other providers working out of the ASC, limiting the group to between 5 and 20 patients per day.
The hospital was also an increasingly bad fit for the complex surgeries the group was now doing on an outpatient basis. The ASC’s recovery area included a row of recliners in which patients were expected to sit for an hour or less before discharge. That was passable for simple cases like carpal tunnel, but not for patients coming out of total knee replacements and spine procedures, who needed more time to recover.
“It really killed our throughput, having patients in those chairs for 3 or 4 hours.”
— Tammy Spohn, OCC administrator
The surgeons decided to build their own facility, the Orthopedic Outpatient Center (OOC), so they could see more patients and provide first-class care in a premium environment. CEO Len Alison had worked with the Virginia Mason Institute on similar projects earlier in his career, and he knew our expertise in Lean facility design would benefit this one.
“We wanted our center to be innovative and intentional from top to bottom, and that meant thinking about flow and efficiency from the very beginning,” he says.
The Solution
Using VMPS and 3P to Ensure Their New Space Enables New Ways of Working
The Institute uses the Virginia Mason Production System (VMPS) in a workshop format called 3P (Production, Preparation, Process) to help organizations define their ideal workflows and patient experience before an architect draws up plans. Facilitators from the Institute guide representatives from across an organization through a series of brainstorms, modeling exercises and simulations. Through this process, the group develops one or more design concepts — consisting of sketches, descriptions and functional narratives for the imagined space. These concepts are later given to the architect to inform the actual blueprints.
“Instead of using a floor plan to figure out how you want things to be, we define how things should be first, and that feeds right into the architect’s design process.”
— Chris Backous, Executive Partner, Virginia Mason Institute
The Institute plans the workshop to align with the needs and expectations of each organization, which in this case meant some unique changes:
- The workshop was entirely virtual, because it occurred during peak COVID-19 restrictions. Instead of a week-long, in-person event, the group met for 3-hour video calls, 3 nights a week for 3 weeks.
- Participants joined from other states and organizations, because the OOC didn’t currently have anyone on staff to represent scrub tech, nursing and other key job positions.
Aligning on Principles, Learning to Iterate
The group’s first task was to align on principles that would guide their thinking. Out of 10 final principles, 2 proved especially influential:
- Exceptional patient and visitor experience
- Exceptional staff experience
These principles spurred the group to innovate in moments when they felt hesitant about a radical idea or gravitated toward a “safer” one.
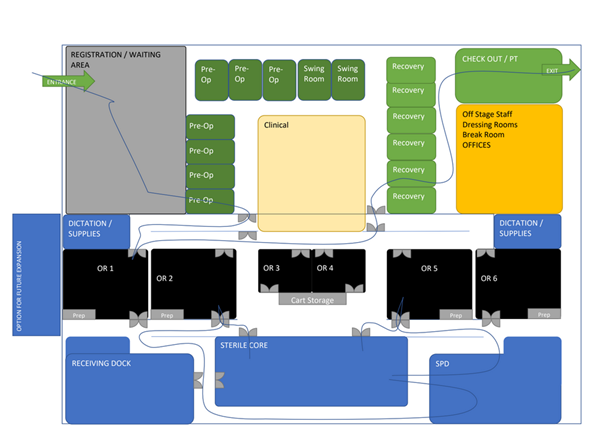
Early sketch of a layout where pre-op and recovery occur in separate rooms, with ORs and staff spaces grouped together on one side of the building. The blue lines illustrate example flow patterns for patients and staff.
For example, during an early sketching exercise, the group envisioned a classic layout where patients go from a prep room to the OR to a recovery room, with nurses and family members following in tow. When they evaluated this layout using their guiding principles, they saw that it created excessive square footage and foot traffic — and was fairly unexceptional from both the patient and staff perspective.
“Then we had the idea of doing prep and recovery in a single room, which unlocked the whole thing for us,” says Alison, the CEO.
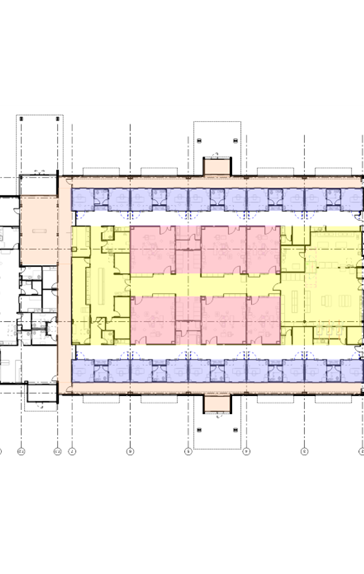
Sketch of the final floor plan, with 10 dual-purpose prep/recovery rooms (purple) lining the outer hallways and 6 OR rooms (pink) in the center, surrounding the sterile core.
They tested their new concept by drawing flow patterns and simulating changeovers and other work tasks with a stopwatch. The benefits were everywhere: Nurses could be dedicated to rooms, cutting down on handoffs that take time and create opportunities for error. Families could relax and stay in one place. The rooms themselves could be invested with features and finishes that make them a comfortable “home base” for patients and visitors.
Further Innovation and Final Concepts
The group came up with numerous other innovations over the course of the workshop, including:
- Passthrough cabinets in OR rooms: The front of the cabinets open into the OR for nurses to access supplies. The back of the cabinets open into the sterile core for staff to stock supplies with less foot traffic and lower risk of infection.
- Soiled linen depositories: Instead of hauling all soiled and trash linens to a single room, staff deposit them in small closets located behind the scrub sinks in the patient-facing hallway. Each patient room is at most 3 doors down from the nearest closet.
By the end of the 3-week workshop, OOC leaders had 3 complete design concepts for their new facility. If anything in their favorite concept proved unfeasible, they had 2 other solutions to fall back on, both of which embody their guiding principles.
As it turned out, they didn’t have to bend on anything. The architect, who had previous experience with 3P, translated the leading concept into blueprints without a hitch. And the contractor, who was adept at sourcing local materials and managing local subcontractors, brought the OOC to life beautifully.

The Results
A Truly Exceptional Facility and Experience
The project was completed on time and on budget. The 3P workshop gave the OOC a detailed vision that helped the group avoid surprises, sacrifices and expensive change orders.
The OCC welcomed its first patient in July 2023 and is steadily building momentum.
- 6 ORs all to themselves
- 10 patient rooms and capacity for 50 patients per day
- 5 additional surgeons and a complete roster of nurses, MAs and other staff
The flow and experiences inside the building are even better than they imagined.
- Patients feel cared for by the convenience and warm, welcoming atmosphere of their prep/recovery rooms.
- Staff rave about the passthrough cabinets and other thoughtful touches.
- Leaders are tracking and optimizing various work tasks and processes to figure out how to make best of the facility.
- Turnover efficiency is already superb, with a team of 4 recently turning over an OR for back-to-back total knee replacements in just 18 minutes. “Twenty minutes is the gold standard,” says Spohn. “So 18 is like a land-speed record.”
Why partner with Virginia Mason Institute?
- Emphasis on form following function – We help organizations define how they want things to work and create spaces that make that vision possible.
- In-depth experience with healthcare and design – We know flow inside and out and speak the language of construction and codes, helping you devise innovative concepts that actually get built and protect your budget.
- Creative thinking that lives beyond the project – Participants carry the brainstorming and test-and-learn habits they develop in 3P into their daily work, turning new spaces into improvement labs where quality and efficiency are examined and enhanced on an ongoing basis.