Case Study | 30 Minutes to 2 for Prior Authorizations: How Training Inspired New Confidence and Led to Systemwide Improvement
At a Glance
The Organization
North Shore Physicians Group (NSPG) is an affiliate of Salem Hospital and a member of Mass General Brigham. The largest multi-specialty group north of Boston, NSPG has more than 350 health care providers in 27 locations. The organization has worked with Virginia Mason Institute to help develop and maintain their system-wide management and improvement method.
Key Decisions
- Adina Trombley, now a Senior Process Improvement Specialist with NSPG, enrolled in the remote Advanced Process Improvement (APIT) training course through Virginia Mason Institute.
- Trombley used her training to pinpoint problems with NSPG’s process for medication prior authorization and present her findings to senior leadership.
- During a two-day improvement event held after the training, the team discovered an unused prior authorization tool within their electronic medical record system and incorporated it into a new process.
Key Results
- Completion of medication prior authorization forms now takes 2 minutes rather than 30 minutes.
- Wait times for responses from insurance providers take less than 1 day, down from 5 days.
- The improvement has rolled out across NSPG and will continue to spread as NSPG signs on more locations.
- The reduced burden of work significantly improved staff morale.
- Visibility on medication costs and shorter waits to treatment improved patient experience.
The Context
Frustrating, everyday tasks contribute to burnout
Burnout continues to be a big problem in health care. It can lead to staff turnover, negatively impact patient experience and even jeopardize the quality and safety of care.
Burnout often stems from stressors related to patterns in the way teams and organizations work. Recent Medscape data identified bureaucratic tasks as one of the top three contributors to health care burnout.
At NSPG, prior authorization (PA) for medications was one of those tasks. Trombley decided to focus on the PA process for her APIT “fieldwork” in which trainees apply their new tools and skills toward real improvements in their workplaces.
“In my previous life I was an administrative staff member in an office setting who sometimes handled prior authorizations for medications. I always wondered why we didn’t have a standard, straightforward way to do them,” she says.
The Challenge
Recapturing the valuable time wasted during prior authorizations
Trombley knew from experience that improving the PA process would eliminate waste and boost both staff and patient experience.
She received coaching and feedback from partners at the Institute as she applied improvement tools from her training to measure and observe NSPG’s medication prior authorization process. Among the findings: the process cycle time was 30 minutes, and there was a lot of variation in the way the task was performed. For example, the MAs had no single, up-to-date source for their providers’ National Provider Identifier (NPI), which is required on all prior authorization forms. Some MAs used an outdated provider list; others looked on NSPG’s intranet; and others searched on Google.
“PAs were a rock in everyone’s shoe,” recalls Trombley. “People were doing this task 13 different ways, and none of them were easy.”
The Solution
North Shore Physicians Group tackles the challenge
Trombley and the staff earned a big first win by creating an NPI Cheat Sheet that lists all current providers and their NPI numbers and posted it at every workstation. She developed the spreadsheet using a strategy called 5S, which helps teams redesign a space or process so it is straightforward, visual and consistent.
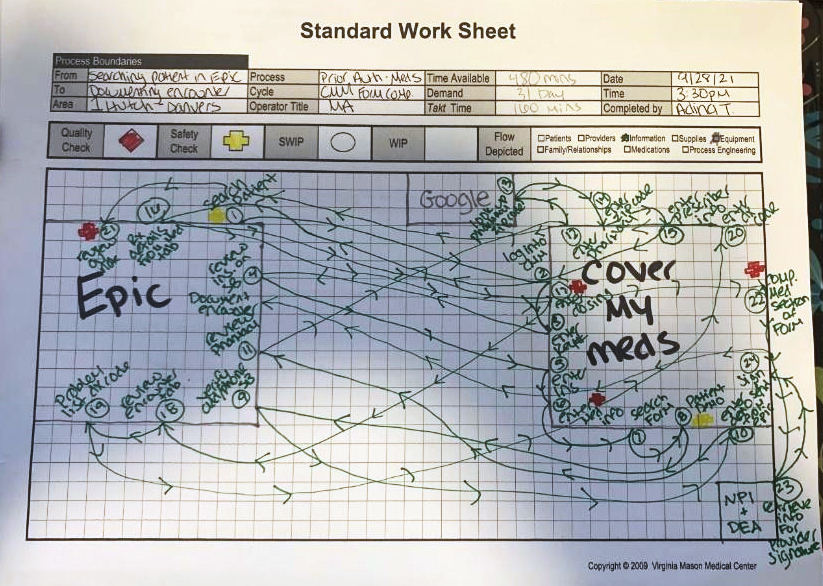
Next, Trombley carefully documented the current state of the medication prior authorization process using other tools from the APIT training. A spaghetti diagram worksheet mapped each step MAs were taking to complete a medication prior authorization. A value stream map measured the cycle time of those steps, and detailed each input and output and who performed them. The visual nature of these tools clearly highlighted the challenges within the process: variation, long lead times and non-value-added steps for staff and the patient. With these results in hand, Trombley had the confidence to communicate with executive leadership.
“Our VP’s eyes nearly popped when she saw my chart showing how many clicks an MA had to do for a prior authorization,” she recalls.
From there, Trombley had the green light to lead a two-day improvement event. During the event, the team researched technology solutions that might support prior authorizations — and discovered that their electronic medical record (EMR) had a built-in tool that wasn’t being used. After confirming that it would work for retail medications in the clinic setting, the team worked to incorporate the tool.
Now, when a provider places an electronic order for a medication, the system uses data within the EMR to pre-populate a prior authorization form with patient-specific insurance information and sends it to the MA. The tool also provides information at the point of care about how much a medication will cost based on a patient’s insurance coverage.
“Without the two-day event we would not have even known this tool was an option,” notes Trombley.
The Results
‘Happy tears’ of relief
Trombley’s advocacy and guidance led to changes that save time, eliminate waste, and improve the experience of both staff and patients:
- The new process takes about 2 minutes of an MA’s time to complete, rather than up to 30 minutes.
- The turnaround time for getting a response from insurance providers decreased from 5 days to just one day.
- Within 30 days of Trombley completing the APIT course, 2 departments at NSPG were already live with the new process. Within several months, all 27 NSPG locations were live with the new process.
- Staff morale improved due to the decrease in the burden of work.
- Patient experience improved because they can get immediate information on the price of a medication and there is a much shorter wait to begin treatment.
“Our clinical staff have been so overworked, and the additional frustration of indirect work can overwhelm the satisfying aspects of their jobs,” Trombley says. “Hearing the MAs talk about the impact of the new process brought happy tears to my eyes. It feels good to know that we’ve made a common task so much easier to do.”
Trombley received a promotion to Senior Process Improvement Specialist and has already taken on new challenges. She recently participated in a two-day improvement event aimed at lessening the strain of new hire onboarding and making sure new employees feel successful in their roles with an eye toward improving staff retention and avoiding burnout. She also recently led an improvement event on Infusion Medication Prior Authorizations.
“I had fun and learned so much from our coach, Rhonda Stewart, and the other seven students in my cohort,” says Trombley. “I had done other training before, but during APIT I dove into the tools and gained a much deeper understanding of how to use them and how to explain them to others. Now I have the confidence to advocate for changes that improve my colleagues’ work.”
Why train with Virginia Mason Institute?
- Immediate results — Our training programs focus on creating immediate results while supporting broader changes that systematize and sustain learning and improvement.
- Personalized coaching — 1-on-1 virtual coaching and feedback helps students apply new tools in real time.
- Intimate cohorts emphasize peer-to-peer learning — Small cohorts in a virtual setting spark group interaction and expand networking opportunities.




