How an Improvement System is Helping North Shore Physicians Group Manage COVID-19
Our recent blogs have focused on stories of how we have used our management system, the Virginia Mason Production System® (VMPS) during the COVID-19 response at Virginia Mason. Today’s blog features one of our first transformation clients based in Salem, Massachusetts. Here we learn of their amazing use of continuous improvement methods to return to daily outpatient operations following a response to surging caseloads during the initial days of the COVID-19 crisis.
Our goal when we engage with organizations is to leave them ready and able to address the challenges of daily operations as well as crises such as the COVID-19 pandemic. We are thrilled to share how North Shore Physicians Group (NSPG) and North Shore Medical Center are embracing their new normal with a problem-solving ability borne from using the tools, methods and training of VMPS, as they continue to learn from Virginia Mason Institute and make this highly effective management method their own.
“In one week, 625 providers and staff were trained and 21 office-based simulations for patient flows were held, successfully readying all teams to see their first patients under the new conditions.”
Implementation:
- Daily management huddles
- Leader rounding
- Production boards
- Plan-do-study-act (PDSA) improvement cycles
- Virtual improvement workshop (kaizen event)
- Office-based simulations for patient flows
Outcomes:
- Patient care flows (lead times) brought into compliance with new infection control blueprint,
- Tools developed to measure, monitor and predict PPE levels required
- Building-by-building plans for safe operations and needed education and training programs developed and deployed
- In one week, 625 providers and staff trained and ready to see patients under new conditions
During the second week of March 2020 as COVID-19 declared a foothold in Massachusetts, NSPG transformed all in-person patient care operations in 29 office locations to remote care. Out of concern for public safety and in accordance with the Massachusetts State stay-at-home guidelines, staff and providers were sent home to work virtually. Like many outpatient care provider groups across the globe, the team had to develop competency at something they had never done before – deliver comprehensive virtual care safely to both COVID-19 and non-COVID patients, all at a greatly accelerated rate. The team also had to build face-to-face patient COVID Care service lines, sorting symptomatic patients to highly skilled clinicians serving in a rapid cycle drive-through testing center, a respiratory illness clinic and a home visit program for the homebound.
As community prevalence of the virus rapidly escalated, outpatient physicians and nurses volunteered to join their inpatient peers to care for the surging inpatient populations at North Shore Medical Center’s Salem Hospital. Surge hit the team in April with expansion of Intensive Care Unit beds from one 20-bed unit to three units, including two that were converted from general medical/surgical units to ICUs, while COVID-19 daily patient inpatient volume topped 140. Ventilator capacity was challenged, and the hospital relied on daily transfers of critically ill patients to other Mass General Brigham hospitals in Boston during the height of impact.
In order to satisfy multiple competing healthcare delivery priorities during the surge and to assimilate the Mass General Brigham Blueprint for Infection Control guidelines into clinical operations during reopening, NSPG leaders and clinicians recognized the need to rapidly develop standard work to ensure delivery of the same high-quality care they are known for, both in person and via virtual connections with patients. Having leaders and clinicians certified in their lean management method based on VMPS allowed for rapid development and deployment of standard work.
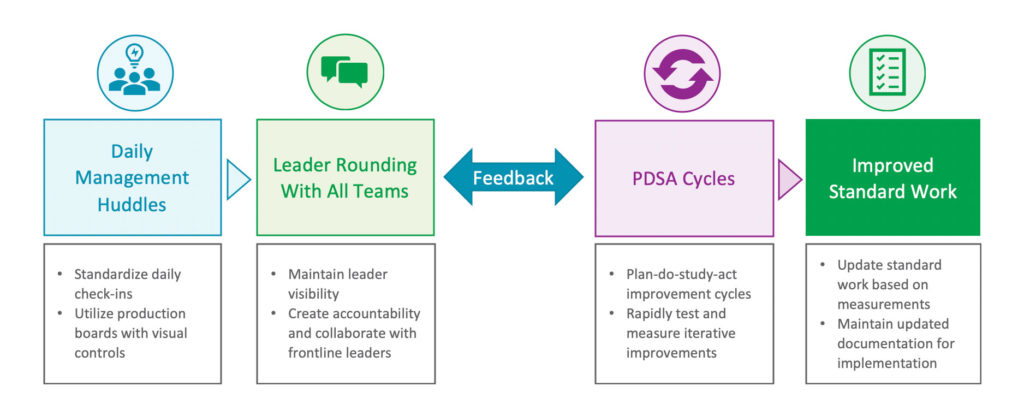
Daily management huddles and leader rounding to all genbas (where the work happens) served as the channel for feedback on what was working and what needed further attention and PDSA (plan-do-study-act improvement cycles). Sharon Lucie, Vice President of Operations for NSPG shared with me that, “Everyone knew that new or improved standard work was needed and knew how to get it done. They also knew from their training that regular observation and measurement along with meaningful visual controls to track performance would be vital to our success with COVID-19.”
As hospital volumes of COVID-19 patients receded in mid-May and community COVID-19 cases sustained a 14-day decline, it became clear that it was safe to enter Phase One of the Massachusetts Reopening Plan. In-person patient access to all offices was slowly reintroduced, the initial focus on patients with urgent medical conditions and now in Phase Two, patients with chronic diseases and all other healthcare needs. COVID Care clinic locations were maintained in parallel, with an emphasis on preserving the COVID-19 patient cohort for clinical expertise, ease of access and patient safety.
Although patient screening standards were introduced and trained at inception, the return to NSPG offices with in-person patient care necessitated careful calculation of personal protective equipment that was in exceptionally short supply, the adoption of MGB Blueprint for Infection Control guidance to create clear infection control measures in the environment, schedule and other changes to create patient and staff social distancing and new clinic flows to support the clinical and operational plan.
“Everyone knew that new or improved standard work was needed and knew how to get it done.”
Sharon, other senior certified leaders and a group of seasoned KPO members determined that at least one kaizen event (multi-day improvement workshop) was needed to address these concerns quickly. Providers and staff who were not deployed to support hospital care delivery had been working from their homes so how were they going to safely gather to address all that they needed to address? They determined that it was time for a virtual kaizen event that brought together over 50 people from North Shore Physicians Group and North Shore Medical Center. Four groups were formed to address safe clinical care delivery, physical plant and PPE readiness, creating effective operational plans and meeting the rapid cycle education and training needs of the returning care delivery workforce. Once Project Forms were developed and desired performance targets were identified, this mighty team logged onto Microsoft Teams and set to work.
Over a two-day period, patient care flows (lead times) were brought into compliance with the new infection control blueprint, tools were developed to measure, monitor and predict PPE levels required, building-by-building plans for safe operations and needed education and training programs were not only developed but deployment began. In one week, 625 providers and staff were trained and 21 office-based simulations for patient flows were held, successfully readying all teams to see their first patients under the new conditions. PDSAs occur daily to maintain alignment to safety and performance requirements as well as to incorporate new guidance which continues to emerge at a rapid pace.
Congratulations to all who are using lean management methods, like VMPS, to return to perfecting the patient experience. You are truly valuable partners in our journey to transform health care.
Webinar | Leadership Through Crisis Interview Series – Sue Anderson and Eli Quisenberry
Want to learn more about how to successfully empower your teams to lead improvements during these challenging times? Watch or listen to our interview webinar – the second in our “Leadership Through Crisis Interview Series” featuring Virginia Mason President, Sue Anderson, along with Eli Quisenberry, director of Virginia Mason’s Kaizen Promotion Office.
Learn more







