Achieving 10-15% Cost Reduction Through Thoughtful Facility Planning
A client recently requested our assistance in redefining how facilities are developed within their organization. In sitting down together, their C-suite shared that it had been reviewing prior capital projects and were keen on preventing cost escalation that result in millions of additional dollars and time due to late-stage development changes. Such expenditures are often linked to supporting care delivery without a clear, articulated vision for how care will be delivered. Failing to declare a “True North” future state for care delivery before design or construction begins can lead to unanticipated fixes, necessary to fulfill the plan. Like many in health care today, the client, was seeking a better way to develop facilities that work for them now and in the future.
The leaders understood the opportunity to do things right and agreed to run a facilitated 3P (Production Preparation Process) workshop. The workshop focused on designing breakthrough, future state care delivery processes along with creating concepts and principles for guiding facility design. This would offer the flexibility and adaptability they wanted to avoid the costly changes of the past. Leadership pulled contributors from across the organization to participate, including executives, administrators, and back-office staff who interact with patients in care delivery space each day. We find that 3P teams comprised of participants across the care continuum produce better results.
During the week-long workshop, the team declared that spaces should:
- allow for collaboration across teams and disciplines
- allow for “heads down” time when needed
- be flexible enough to ensure 75% or better utilization as defined as patient in room with providers (a goal of patients sitting alone in rooms for no more than 5 minutes was established)
- support onstage (with/for patients) and offstage (without patients) work flows
- …and so much more!
Designing breakthrough
Whole clinic design concepts created by the team reinvented the traditional waiting room space into an arrival and engagement space that welcomed all arriving patients into an experience tailored to their individual needs. High volume, high frequency services were located together and separated from those spaces designed for supporting behavioral health needs.
All team members agreed that new space alone would not solve the problems that were causing staff burnout and patient dissatisfaction. They knew that these new facility designs must emerge from exceptional patient and staff experiences. Future state care delivery processes developed by the team ensured that:
- patients would not wait from one provider to the next.
- data were gathered at the right time and fed forward into the process.
- team members were able to work at the top of their license and talent ability.
- care would be delivered as a team versus the traditional team member to team member handoff method.
- care would cross the delivery silos so that a patient could receive medical, behavioral health, dental and pharmacy support care in one visit.
Creating concepts and principles
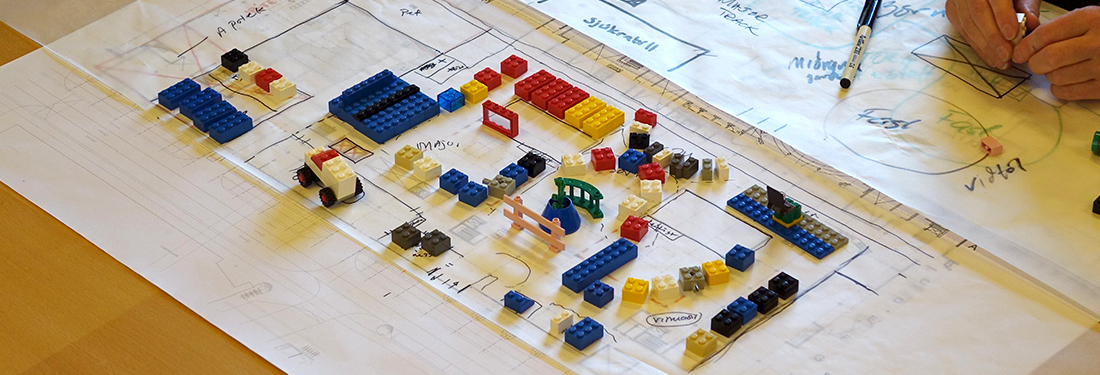
Through the 3P workshop, the team was able to reduce the patient’s lead time (time in clinic from arrival to departure) by 40% through better synchronization and coordination between care teams using the VMPS Flows of Medicine®. One of the methods used during a 3P workshops is rapid space prototyping. The team harvested pros and cons through this method and arrived with a set of facility layout concepts and guiding principles that could apply to any facility project in the future, regardless of the size and scope. By determining future state care delivery prior to design and construction of a new facility, the team hopes to prevent cost overruns valued at 10-15% of the total construction cost. Developing the facility design guiding principles and declaring the vision for care delivery processes has empowered this organization to optimize its people and financial resources with breakthrough approaches for meeting and exceeding their patients’ expectations. I look forward to seeing their great work come to life with the first facility planned for later this year.
The patient’s lead time, or time in clinic from arrival to depart, was reduced by 40% through better synchronization and coordination between care teams using the VMPS Flows of Medicine®.
Designing future state care delivery process
When you design a health care facility based upon how you work today, you ensure that your space will need revisions as your care delivery model evolves. Care delivery can change so quickly that major space revisions might occur before you occupy the new space. Planning and future-proofing facilities by designing with flexibility and adaptability in mind is the key to prevent spending beyond budget.
Our Virginia Mason Institute team works with a very simple rule carried forward from years of developing new spaces at Virginia Mason Hospital — “no new space without new process”. At the start of any new facility design effort, it makes sense to seize opportunities and create new ways of providing the highest quality patient care by eliminating the waste that creates burden of work for our teams and less than ideal experiences for our patients.
Cost-effective, breakthrough facility design using our proven 3P methodology begins with engaging the people who do the work to envision how to best do the work and letting these future state care processes inform space. In this way, form will truly follow function.
Virginia Mason Institute’s proven approach to breakthrough development using 3P tools and methods can help you go further with any effort, whether your organization is exploring new facilities, planning significant upgrades, developing new service offerings or setting new strategic vision for all or parts of your organization.