5 Tactics to Break Down Silos and Support Cross-Functional Collaboration
The Challenge: Inefficiencies continue to plague healthcare due to silos that harm morale, financial performance, and patient experience
What are silos?
Organizational silos are separations based on department, specialization, or location. While it might seem logical to keep teams separate and distinct from each other, the business world has long acknowledged that silos create misunderstanding, inefficiency, and unnecessary competition across departments. Teams perform better when you break down the barriers and create a culture of collaboration in information, responsibility, and vision.
The discussion around de-siloing healthcare often centers cooperation (or lack thereof) among clinical providers, giving rise to the popular concept of care coordination. However, these silos also exist in the operational context of staff scheduling, room availability, billing, admitting, and other system functions.
Each department has its own budget, its own way of doing things that are unknown to other teams, and a manager who does not like loaning out ‘their people’ to anyone else. As a result, when one department is slammed, medical assistants in another department might be sitting idle and unable to help because they don’t have the training or information necessary to lend a hand. De-siloing can be the solution for these unnecessary barriers between staff in different departments, thereby making a more cohesive healthcare team.
Five tactics for collapsing silos
Leaders in the Virginia Mason Franciscan Health (VMFH) system have found that although waste, errors, and tribalism were evident among floor and cubicle staff, the root causes lay at the level of management. Separation and limited communication between managers in different departments set the tone for the staff. So when it came to devising a solution, managers were the ones who had to come together.
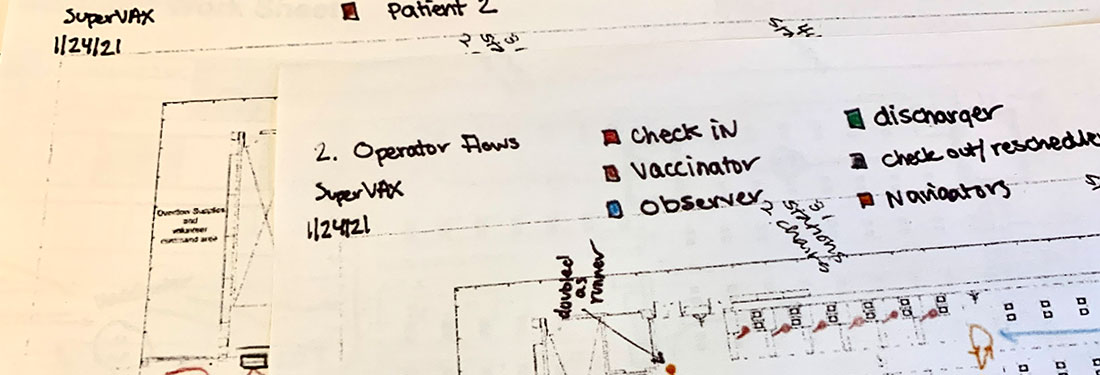
Local leaders hosted improvement events known as Rapid Process Improvement Workshops (RPIWs). These workshops brought together managers and team members in Patient Financial Services (PFS) and Virginia Mason Federal Way Medical Center, one of the system’s outpatient clinics. Through collaboration the attendees of RPIWS were able to figure out a solution.
In fact, they were able to devise a number of several complementary tactics that created a new solution system. In the case of PFS, it took multiple RPIWs over multiple years to arrive at and implement all the reforms. These reforms took time and effort, but have since helped break down the silos that got in the way of smooth, effective workflows and, in some cases, optimal patient care.
After adapting the wisdom gleaned over years of improvement efforts, we have identified five tactics that can help address siloing-related problems that many health systems experience today. In what follows, we explain each tactic and how it has positively impacted our work.
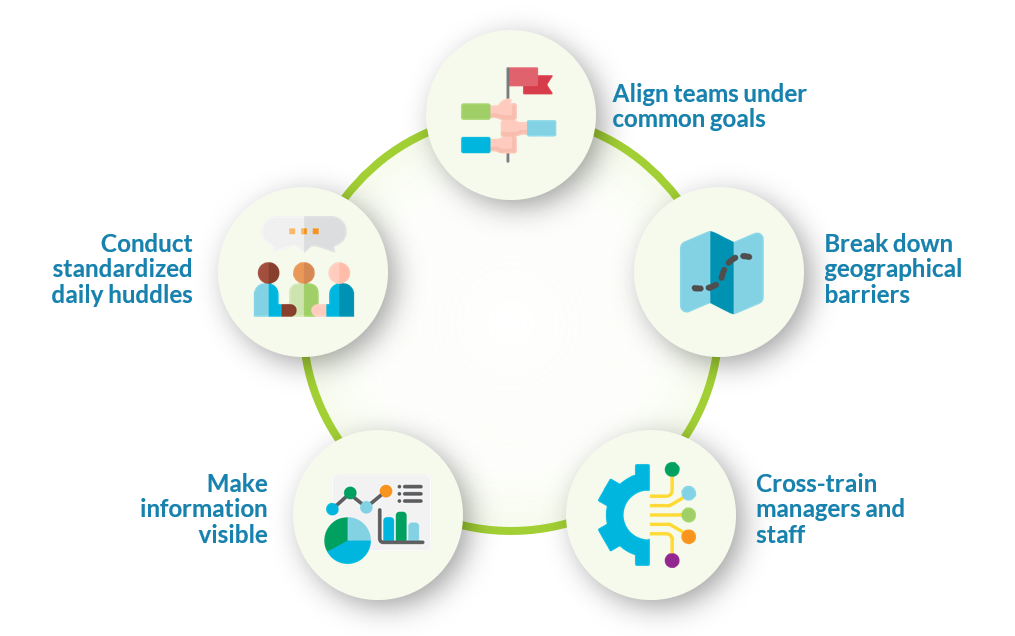
Align teams under common goals
Team-specific goals are important, but they should not be paramount. Teams should work towards one or more shared goals with metrics attached to that vision whenever possible.
The problem with separate teams pursuing separate goals became clear to the PFS team. The emphasis on team-specific metrics, such as how fast you get a patient through the arrival process, was one reason that the entire PFS department was performing poorly in one of its main metrics: days revenue outstanding, or the DRO. Team members in other departments were creating defects in patient information due to their focus on speed – which was the paramount priority for their individual team.
The solution was encouraging cross-departmental management to align teams under the shared goal of having a strong bottom line. If the PFS had a good month, that was everyone’s victory. If it had a bad month, that was everyone’s responsibility.
Teams still have local metrics, but the DRO became paramount. Managers agreed to measure their teams against that number first and foremost, and by doing so PFS managed to lower the DRO from 29.7 to 28.6, which at the time was a new department record.
Break down geographical barriers
Physical distance inhibits collaboration, which might seem contrary to the logic that grouping teams as independent units is more efficient. By organizing the work space so that departments that frequently collaborate are proximal to each other, each department is more likely to step out of their silo and act as an interdependent part of a bigger group.
For example, different teams within PFS reformed their geographic structure so managers of these teams work in the same physical space — a large open cubicle space shared by the managers and dubbed the Nexus.
Soon after implementing the Nexus, managers were spending 15 percent more time on their unique managerial duties as opposed to correcting errors and resolving breakdowns in their teams’ workflows. The collaboration among managers was so effective that an entire full-time manager role — an unfilled job posting at that time — was eliminated, saving the hospital from paying an additional manager salary.
Breaking down geographical barriers is also a fundamental for optimizing the clinical environment through flow stations. You can learn more about those best practices in our free on-demand webinar: Fundamentals for Improving Flow in the Ambulatory Setting.
Cross-train managers and staff
The ability to call on someone from another team when any team member needs help allows all teams to perform at their best. On the other hand, when teams are in silos, they can have days or weeks where they are overworked and understaffed and there is nothing anyone can do to help.
In PFS, managers were cross-trained prior to moving into the Nexus together. Even without a shared space, they quickly learned how to use their new shared skills and help each other as needed. Their flexibility paid enormous dividends — eliminating the need for three full-time manager positions, reducing overall manager hours by 19 percent, and reducing managers’ negative/neutral feelings about their jobs by 41 percent (as shown in an internal survey of manager morale).
Cross-training was also instrumental to improving overall work in Federal Way. Everyone below the manager level is now required to be trained in at least one additional area, as well as learning how to work the phones. As a result, systems are more resilient, even when key team members are unexpectedly absent or called away.
Make information visible
To effectively use the information shared between teams, you need to make it easily accessible to everyone. In a setting as fast-paced and information dependent as healthcare, shared team information needs to be enshrined. Teams across VMFH use a visual management board in a central place where everyone knows to look for reference, whether it’s a live digital dashboard or a physical whiteboard.
Displays like this communicate to everyone on the team what supply and demand look like for the day and make it clear where needs are normal and where they are exceptional. For healthcare providers, having a consistent, easily interpreted breakdown of the day is invaluable for planning and communication. In Lean systems these visual management boards are known variously as production boards, staffing boards, or huddle boards.
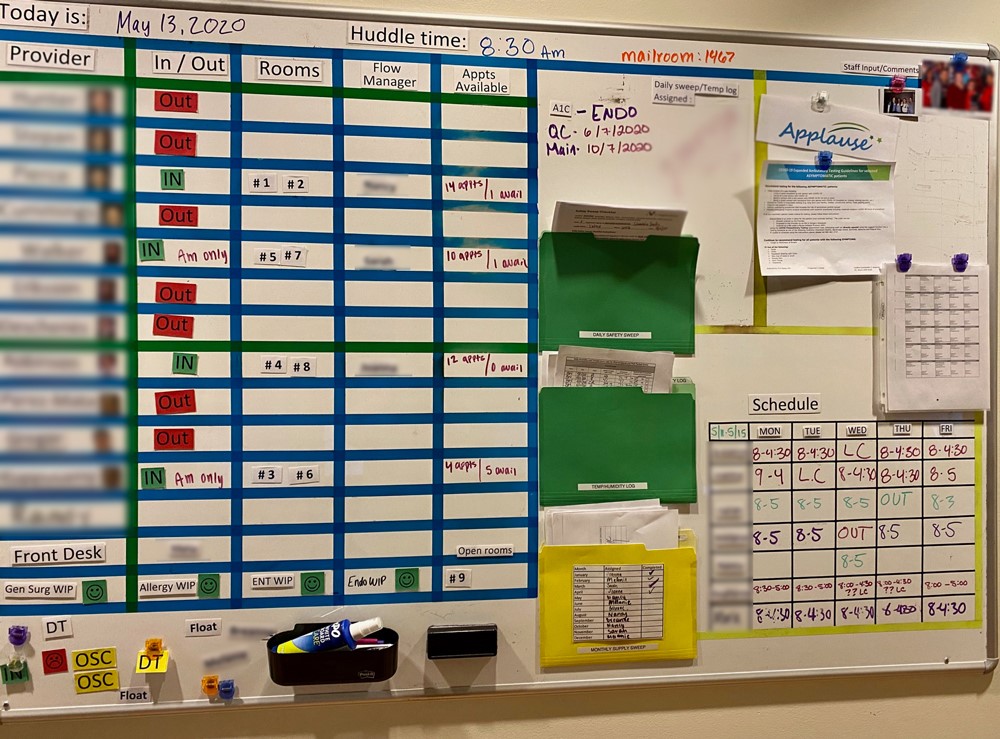
The visual management boards used by teams in Federal Way and PFS account for all information specific to the current day, such as who is working and when they are taking their breaks. They also account for information that applies to every workday, such as which areas each staff member has been trained in, as well as status reports on things like team performance metrics and staff requests that the manager has agreed to follow through on. It is a lot of information, but everyone quickly learns how to navigate the board to figure out what they need to know.
Visual management boards also break down vertical silos by taking knowledge that was previously known only to the manager and sharing it with everyone. This transparency makes potential problems more visible to all team members, creating new opportunities for collaborative solutions.
Other benefits include saving time, because people know exactly where to find the answers to their questions. In turn, we have found this often makes the work environment calmer and quieter. Visual management boards maintain the peace by making visible in one central place what used to be scattered across memos, trapped in people’s heads, and communicated erratically across teams.
Conduct standardized daily huddles
There is a difference between having a daily huddle and having an effective daily huddle. An effective daily huddle follows a standard agenda based on what the team needs to know to do their job that day. This information is also displayed — and updated throughout the day — on the board for teams to refer to.
At Virginia Mason Federal Way teams would huddle in the morning, under manager direction but without a set structure. The manager would cover general announcements rather than actionable information such as who was out sick and how to plan for the day. As a result, the team spent the first hour after the meeting figuring out what needed to be done and scrambling to do it. In the words of clinic manager Latrice Bowles-Reynolds, “From the very beginning of the day, it went downhill. And there was no getting out of it.”
Now that the clinic in Federal Way has reformed its huddles with a set agenda and focus on action, teams are accomplishing together in five attentive minutes what used to cost them an hour of running around alone. Even better, the team lead, rather than the manager, runs the huddle. This frees the manager to focus on other work and elevates engagement among staff, who feel more control over their day and how they are approaching it. The huddle and the information board create opportunities for members to identify and volunteer the right choices for their team without being asked.
Insights and nuances regarding this approach
Managers are the team members that must change their perspectives and habits the most to break down silos. Instead of prioritizing their own goals or leadership style, managers have to plug into the bigger effort. As such, managers that adopt a team-centric mindset of “How can I help?” will be the most effective at breaking down silos because they will have the attitude necessary to act with the whole organization in mind..
Practices that break down vertical silos like leader rounding and root-cause analysis can feel burdensome at first. It may seem a lot easier to manage from behind the desk. Some managers that prefer a less hands-on approach may have to adapt their style to incorporate modern leadership behaviors that support de-siloed workplaces.
However, we have found that many managers thrive in a de-siloed environment. They work less overtime, feel more supported, have more meaningful opportunities to coach staff and foster growth, and receive more credit for contributing to the organization’s larger goals. The adjustment period that comes with de-siloing will eventually reap long-term rewards through improved communication and efficiency.
It all adds up to a reversal of the axiom ‘culture eats process for lunch’. Meticulous dismantling of literal and mental silos is fundamentally done for the sake of removing waste and improving results. But it also nets a more positive environment where culture and process work synergistically.
Just ask Latrice, clinic manager at Federal Way. She found the transition to de-siloing difficult at first and was not sure it would work. Now she feels differently. “Honestly, it’s amazing,” she says. “It empowers me as a leader to make a difference in the departments that I manage. And it empowers the team. There is structure and engagement that we never dreamed we would have.” By breaking down silos, healthcare facilities can begin to chip away at inefficiencies and create better workplaces that subsequently provide better patient care.
Ready to learn more?
- Watch Rhonda’s “Fundamentals for Improving Flow in the Ambulatory Setting” webinar and learn more about foundational principles, methods, and routines that can help you optimize the clinical environment
- Learn more about the leadership behaviors and practices necessary to empower healthcare teams. Watch the on-demand webinar, listen to the audio, or read the Q&A transcript of “Developing Modern Leaders for a New Era in Healthcare”